Education
- Max-Planck Institute of Molec. Physiol. (Germany)1991PhD
Research
RESEARCH: Recent research data from our laboratory and other research institutions compellingly suggest that in pro-tumorigenic microenvironments finely tuned cooperation between proteolytic and non-proteolytic processes undeniably contribute to an ‘uncontrolled’ invasion and metastasis of malignant tumors. Pursuit of a better understanding of these processes and development of clinically relevant pharmaceutical countermeasures is the long-term research focus of our laboratory.
TRAINING & MENTORING: Our research group is dedicated to building and maintaining a highly collegial and supportive work environment where all personnel can experience open communication, teamwork, and individualized mentoring to help all team members achieve their individual career goals.
The most life-threatening aspects of any cancer are tumor invasion and metastasis. These events are driven by mechanisms regulating cell growth and survival, cell:cell and cell:matrix interactions, cell migration, and those controlling the proteolytic tumor microenvironment (TME). Based on clinical observations, high levels of serine proteinase urokinase-type plasminogen activator (uPA) and its cell surface receptor (uPAR) in TME are positively correlated with a poor patient prognosis in numerous malignancies, including human breast and ovarian cancer. These data seem aiding the widely accepted paradigm that uPA released by tumor cells catalyzes activation of plasminogen to plasmin, which in turn catalyzes degradation of extracellular matrix (ECM), particularly the basal lamina, thus facilitating invasion of disseminating tumor cells into tumor-adjacent tissues. Paradoxically, elevated tumor levels of the physiological most relevant inhibitor of the uPA-system, the plasminogen activator inhibitor type-1 (PAI-1), are significantly associated with a poor prognosis as well, the PAI-1 level, in fact, being one of the most informative biochemical prognostic markers in a variety of human malignancies.
Most interestingly, numerous functions of PAI-1 strongly associate with non-proteolytic mechanisms. Through interaction with an endocytic receptor, LRP1 (LDL receptor-related protein 1), PAI-1 activates intracellular signaling pathways leading to recruitment of inflammatory cells and initiates fibroblast differentiation to ECM-producing myofibroblasts, stimulating a motile program and initiate a cytoarchitectural restructuring (Ref #1). In addition, PAI-1 initiates LRP1-mediated endocytic clearance and subsequent subcellular redistribution of uPA/uPAR and integrins (Ref #5), a family of cell adhesion receptors, emphasizing the functional and regulatory interaction between the cell adhesion and motility machinery and any non-proteolytic activities by PAI-1 and the plasminogen activation system.
WHY CHOOSING OVARIAN CANCER AS A RESEARCH MODEL?
The biology of serous high grade Ovarian Cancer (OvCa) is very different from that of most other solid tumors. OvCa predominantly disseminates into the peritoneal cavity and metastasizes along a transmesothelial route and rarely metastasizes hematogenously. During transcoelomic dissemination, OvCa cells float in the peritoneal fluid and are carried throughout the peritoneal cavity. They attach to the mesothelial lining with a high preference toward the omentum, a double fold of the peritoneal membrane covering the bowels and very rich in fat storing adipocytes.
Floating OvCa cells form aggregates, or “spheroids” to overcome anoikis and avoid immune surveillance. Spheroids have been shown to be diverse multicell-type structures containing cancer-associated fibroblasts, activated mesothelial cells, cancer-associated macrophages, and modified adipocytes (fat storage cells). During their intraperitoneal passage, OvCa cells will use their integrins to attach to the FN/VN-containing ECM secreted to the apical surface by mesothelial cells. Upon attachment, OvCa cells, initiating a still undetermined mechanism, “push/pull” the mesothelial cell layer apart and invade into the underlying tissue.
All these various steps independently have been shown to require PAI-1 either during their initiation or regulation. Individual OvCa cells, multicellular spheroids (including their various resident cell types), and mesothelial cells not only express PAI-1 but also PAI-1 target proteins (e.g., uPA, uPAR, LRP1, integrins (αV, α5, β1), FN, VN, TLR4, TGFβR) and PAI-1 regulated signaling pathways (e.g., PI3K, AKT, TGFβ).
CLINICAL IMPLICATIONS: Ovarian cancer is the deadliest gynecological malignancy in the Western world. Over 75% of patients have metastatic disease at time of diagnosis. Current treatment options include surgical interventions (e.g., debulking surgery or cytoreduction surgery) followed by platinum-based chemotherapies (cisplatin or carboplatin), potentially in combination with taxanes (paclitaxel or docetaxel). However, 50-70% of patients will relapse withing one year. When such relapse occurs, in most cases the OvCa cells have acquired a cisplatin-resistant phenotype with the responsible mechanisms still poorly understood. However, recent new clinical and laboratory data directly incriminate increasing PAI-1 expression in the development of chemoresistance, particularly through modifying cellular functions in those cell types present in the OvCa TME, in floating and attached spheroids, thus determining their subsequent contribution to adhesion, implantation, and invasion.
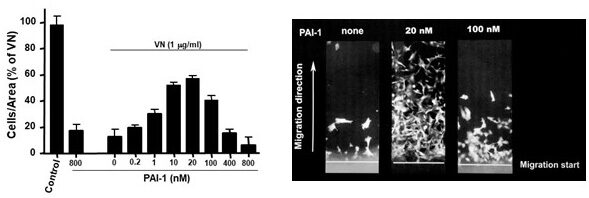
REGULATION OF TUMOR CELL ADHESION, MIGRATION, AND INVASION THROUGH PAI-1:VITRONECTIN INTERACTION
We recently described a novel uPAR-dependent mechanism by which PAI-1 facilitates tumor cell detachment from vitronectin (VN) and other ECM proteins highly expressed in TME and wound beds, e.g., FN, LN, Coll. We found that PAI-1 induces ‘deactivation’ of uPAR and a variety of matrix-engaged integrins, and promotes their LRP1-mediated endocytosis, subsequent recycling, and intracellular redistribution (Refs #6, #10). This novel concept of deadhesive activity by PAI-1 as a proteinase inhibitor suggests a central role for PAI-1 in promoting rapid cycles of cell attachment and cell detachment in tumor cells. This mechanism of increasing the mobility of cancer cells might potentially explain the surprising significance of PAI-1 as clinical marker for poor prognosis and shorter survival in OvCa. Thus, our laboratory is interested in further investigating the functional connection between tumoral PAI-1, VN, and adhesion receptors and its contribution to intraperitoneal OvCa cell attachment and transmesothelial invasion.
Vitronectin (VN) is a multifunctional glycoprotein present in blood and extracellular matrix involved in cell attachment, spreading, migration and invasion. Binding of PAI-1 to VN stabilizes the active, inhibitory conformation of PAI-1. Thus, VN also serves to regulate proteolysis initiated by plasminogen activation. Elevated VN expression has been detected in the TME of invasive tumors, e.g., OvCa, mandating further investigation into pro-invasive functions of VN.
DEVELOPING 3D MULTICELLULAR ORGANOID MODELS FOR TRANSLATIONAL RESEARCH IN HUMAN OVARIAN CANCER (OvCa).
In view of amassed data tightly associating increasing PAI-1 protein expression in human patients’ spheroids with increasing resistance to platinum-based chemotherapy in reoccurring OvCa, this project aims to investigate the following research questions: (1) How does increasing PAI-1 expression support mesothelial attachment of spheroids and the transmesothelial invasion by OvCa cells? (2) How do PAI-1-associated mechanisms, increase tumor cell resistance to platinum-based chemotherapy in reoccurring human OvCa? We are developing and testing single and multicellular in vitro disease models for the subsequent design of in vivo murine models to gain better insights into those mechanisms and pathways. Ultimately, we aim to manifest PAI-1 as a therapeutic target in treatment of chemoresistance in OvCa.
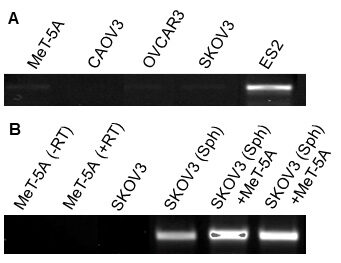
Currently, increasing focus is directed toward the question how autocrine and paracrine mechanisms affect the phenotypes and functions of various cell types in spheroids, prior, during and after their attachment to the mesothelium. In this context, our laboratory focuses on how PAI-1 contributes to either initiating or supporting those mechanisms. Recently, we demonstrated in vitro (see Figure 5) using two human OvCa cell lines either containing (ES2) or lacking (SKOV3) a PAI-1 transcript that cell:cell interaction (e.g., spheroid formation) and subsequent attachment of those spheroids to mesothelial cells (Met-5A; no PAI-1 transcript) progressively leads to increased expression of PAI-1 in those cultures. Experiments are under way to identify the cell type responsible for the increase in PAI-1 expression - cancer cell or mesothelial cell.
Publications
View Ralf-Peter Czekay's articles on the National Institute of Health's PubMed website.
