We do not follow a track-based curriculum. We feel it is important for each resident to have the flexibility they desire as they obtain the experiences and training they require to be successful in their future career goals. Below are examples of what each academic year might look like.
PGY-1
First-year residents focus on building foundational pediatric medical knowledge and patient care skills. As interns, they are supervised by senior residents, fellows, and faculty. They become acquainted with the medical health care system within Albany Medical Center and the surrounding community.
| Rotations | 13 Four-week Blocks |
|---|---|
| Ward | 3-4 |
| Ward Night Team | 1 |
| NICU | 2 |
| ED | 1-2 |
| Ambulatory/Newborn | 2 |
| Developmental and Behavioral | 0-1 |
| Community Health/Acute Care | 1-2 |
| Individualized | 0-1 |
| Elective | 1-2 |
| Four Weeks Vacation | 1 |
| STAR Block | 1 |
PGY-2
Second-year residents graduate into more autonomous roles while continuing to build their medical knowledge and patient care skills. They develop their leadership skills and enjoy numerous opportunities for teaching residents and medical students. Significantly, second-year residents begin utilizing their six individualized block rotations as outlined by the ACGME. These rotations allow residents to tailor their educational experience to meet their own career goals.
| Rotations | 13 Four-Week Blocks |
|---|---|
| Ward | 1-2 |
| NICU Night Team | 1 |
| NICU | 0-1 |
| PICU | 1-2 |
| ED | 1-2 |
| Ambulatory | 1 |
| Adolescent | 0-1 |
| Individualized | 2-5 |
| Ward Night Team | 0-1 |
| Four Weeks Vacation | 1 |
PGY-3
Third-year residents hone their teaching and supervisory skills as they take on more responsibility for decision making and leading their patient care teams. We emphasize independent and critical thinking skills as they approach graduation.
| Rotations | 13 Four-Week Blocks |
|---|---|
| Ward | 1-2 |
| Ward Night Team | 0-1 |
| NICU | 0-1 |
| NICU Night Team | 1 |
| PICU | 0-1 |
| Ambulatory | 1 |
| Individualized | 2-4 |
| Adolescent | 0-1 |
| Elective | 5 |
| Four Weeks Vacation | 1 |
Conferences & Electives
Topics routinely include the following: American Board of Pediatrics general didactics by faculty, ethics, the “Bread and Butter” resident-directed lecture series, house staff meetings, morbidity and mortality conference, or team based learning (TBL), and clinical skills workshops such as suturing, lumbar punctures, and casting and splinting.
Formal Board Review takes place one to two times each block in a faculty-led, small group format. This format emphasizes test taking strategies while reinforcing medical knowledge. Additional board review materials are available to our residents in the form of the MedStudy board review curriculum, and Pedialink online access for independent study during quarterly ILP assignments.
Every resident workshop includes didactics and skills training to develop our residents’ teaching abilities–focusing specifically on giving feedback, evaluating learners and their needs, and modeling clinical reasoning. The workshops dovetail with two subsequent experiences. The first is our unique Learning to Teach Blue Senior ward rotation. The second is our longitudinal resident-delivered lecture series beginning with “Bread & Butter” lectures by PGY-2s aimed at new PGY-1s and culminating with a series of “Case Management” presentations by PGY-3s emphasizing critical thinking and concise delivery of focused didactics as they review cases they have worked that year.
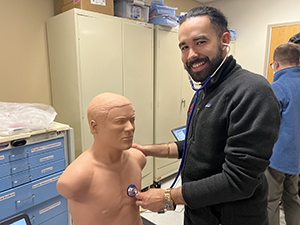
We are fortunate to have access to a state-of-the-art simulation center within the medical college. We use the Sim Center routinely for NICU Boot camp curriculum, monthly mock codes, the “delivering bad news” workshop with standardized patients, and conducting our bedside ultrasound curriculum.
Longitudinal learning is strongly emphasized at Albany Medical Center in the form of Individualized Learning Plans (ILPs), YALE Team Based Learning (TBL), and the Quality Improvement (QI) curriculum.
ILPs are tailored to the adult learner and encourage residents to actively design and execute their own longitudinal road map of their studies. The program schedules biannual “ILP Round-Ups” in which residents meet with their ILP advisor for 5-15 minutes to reflect on their success from the past six months and plan for the next six months. Residents are also expected to meet with the ILP coaches between these scheduled meetings as needed to optimize their study efforts throughout residency.
YALE TBL occurs once a block and is led by a PGY-3 and PGY-2 resident with our Gen-Peds faculty functioning as discussion moderators. Residents receive readings prior to these scheduled conferences and then work in small groups to answer questions and discuss clinical points. The faculty draw on their years of practice and expertise to provide clinical pearls and nuanced answers and approaches to challenging clinical scenarios.
All PGY-1s complete Institute for Healthcare Improvement modules during their acute care rotation and take part in our flipped-classroom Team Based Learning QI experience during their PedSTAR block. All residents then commit to projects (often as multi-year teams). The faculty and resident teams then present their data and their progress at quarterly “Quality Management” conferences.
Our program will help you develop elective experiences above and beyond the required experiences that best prepare you for your career goals.
- Anesthesiology
- Adolescent II
- Bioethics
- Camp Elective
- Cardiology I & II
- Caregiver Elective
- Chief Elective
- Circumcisions
- Community II
- Dermatology (Self Study)
- Development and Behavior II
- Endocrinology
- Pediatric Emergency Medicine III
- ENT
- General Peds- Academic
- General Peds- Private
- Gastroenterology
- Genetics/Metabolism
- Hematology/Oncology
- Hematopathology
- Hospitalist Elective I & II
- Infectious Disease
- Lactation Medicine
- Nephrology
- Neurology
- NICU Elective
- NICU Transport Elective
- Nutrition
- Ophthalmology
- Orthopedics
- Palliative Care
- Surgery
- PICU Elective
- PICU Transport Elective
- Psychiatry
- Pulmonology
- Radiology
- Research Elective
- Rheumatology
- Sedations
- Sports Medicine
- Ultrasound Elective
- Urology
Mock Codes
We are fortunate to have access to a state-of-the-art Patient Safety & Clinical Competency Center (PSCCC) in the medical college. We use the Sim Center to routinely deliver the primary component of our pediatric mock code curriculum. Our pediatric mock code committee, led by our intensivist, Dr. Shahi Ambati, delivers approximately six pediatric “mega codes” to each resident throughout their three year training experience. Four residents are chosen on a bimonthly basis, and are excused from clinical duties to attend. They arrive at the PSCCC, complete a pre-survey, proceed through an ABP validated code scenario, debrief with Dr. Ambati, and then run through the code a second time. These sessions are designed to expose residents to emergent code scenarios while also allowing them to practice hands-on and communication skills. The session concludes with a post-survey to evaluate the resident experience and knowledge retention.
To augment the mega codes in the PSCCC, the Learning to Teach Blue Team Senior is tasked with administering one to two mini mock codes during their respective rotation. These scenarios emphasize recognition of common, acute crises scenarios as well as clinical decision making, and communication skills. Additional mock codes are performed in the NICU for common NICU code scenarios.
Ultrasound Curriculum
Diagnostic ultrasound is the future of clinical practice. As part of our simulation curriculum, along with mock codes, the giving bad news program, and procedure workshops, we developed one of the first courses in bedside ultrasound skills in general pediatrics. Since 2017, all of our residents have undergone 24 hours of structured teaching in how to use ultrasound diagnostically and to place PIVs beginning in intern year. Our trainees have the chance to use their skills in the NICU and PICU to address clinical problems and support bedside procedures.
NICU Bootcamp
Vent Workshop
Masters in Bioethics
The Alden March Bioethics Institute’s online Master of Science degree in bioethics provides mid-career professionals in public health, pastoral care, patient advocacy, medical social work, medical research, and the life sciences with innovative and challenging training in bioethics.
The program at Albany Medical College can be completed entirely online, giving students the flexibility to work on courses according to their schedule. Each online term is 10 weeks and the program features rolling admissions with four terms per year. The winter term begins on Nov. 30.
Qualified Albany Medical Center employees are eligible to receive a Trustee Scholarship to offset 50 percent of tuition cost. A bachelor’s degree is required for admission into the program. Learn more here or contact Alexandria Busch, manager of administrative operations at the Alden March Bioethics Institute, at [email protected] or 518-262-9396 for more information.
| Weekday | Morning schedule | Afternoon schedule |
|---|---|---|
| Monday | Morning Conference: 8 a.m. | Noon Conference: 12 p.m. |
| Tuesday | Grand Rounds: 8 a.m. | |
| Wednesday | Morning Report: 8:30 a.m. | Noon Conference: 12 p.m. |
| Thursday | Morning Report: 8:30 a.m. | Noon Conference: 12 p.m. |
| Friday | Case Management: 8 a.m. |
PedSTAR
Every spring, we excuse all of our PGY-1s from their typical clinical duties and to participate in our Pediatric Scholarly Track for Advocacy and Research (PedSTAR). This is a four-week experience during which all interns receive:
- One week of intensive advocacy training drawing on the expertise of several pediatric faculty while leveraging advocacy opportunities that exist in the state capital of New York.
- One week of hands-on instruction in developing clinical research skills. This week is comprised of multiple mini didactic sessions including but not limited to how to write an IRB proposal, grant proposals, consents, and data analytics.
- One week dedicated to training in quality improvement, leadership and teaching skills, and simulation.
The block concludes with each resident committing to designing either a research or advocacy project to complete in the following two years of their training. The final week of the block is used to draft an IRB proposal or a roadmap for their advocacy project in a series of small group workshops.
Each resident will present their project at our annual internal residency research day, a national or regional conference, and during our annual PedSTAR Grand Rounds in the spring of their third year.
PedSTAR (Pediatric Scholarly Track for Academics and Research) was developed in 2015 to provide:
- Basic research education delivered by basic science and clinical research faculty at Albany Medical Center
- Choosing a project
- Research design
- Literature search techniques
- Bibliography management
- IRB proposals
- Statistical planning
- Scientific writing
- Presentation skills
- Protected time for creating, developing, and completing a resident-led project
- Workshops
- Project design
- Abstract writing
- Presentations
- Support for research elective blocks
- Resident-led goals and objectives
- Approved by research mentor
Year One:
- Two full-day conferences for PGY-2 and 3 in research track
- Lectures and workshops
Year Two:
- Three full-day conferences for PGY-2 and 3 in research track
- Lectures and workshops
- Follow-up sessions in PGY-3 year
Year Three:
- A full protected week for entire PGY-1 class with basic research education
- Lectures
- Writing workshops
- A second protected week for PGY-1 residents who choose a research track
- Project specific workshops
- Guided independent time to:
- Create a bibliography in a reference manager
- Meet with mentors to design a project
- Meet with statisticians to determine best statistical design and tests
- Meet with IRB staff, then write and submit IRB proposals
Research Productivity:
- Poster presentations at academic conferences
- Platform presentations at academic conferences
- Publications
Class of 2013: 20% of pediatric residency
Class of 2016: 70% of pediatric residency
Our residents receive continued mentorship and guidance from the PedSTAR faculty throughout residency in the form of annual “Round-Ups” as well as in preparation for the pediatric conference season each spring. Residents receive guidance on navigating submission processes, poster design and presentation, and how to write abstracts and articles. Residents are encouraged to partner with faculty throughout the children’s hospital to facilitate projects that best suit their interests. The PedSTAR faculty can function as consultants to help guide research and advocacy projects using best practices.
Research
Amy Mitchel, PharmD
Simulation Workshops
Sarah Klaiber, DO